Ley, R. E., Peterson, D. A. & Gordon, J. I. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell 124, 837–848 (2006).
Google Scholar
Scher, J. U. et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife 2, e01202 (2013).
Google Scholar
Nii, T. et al. Genomic repertoires linked with pathogenic potency of arthritogenic Prevotella copri isolated from the gut of patients with rheumatoid arthritis. Ann. Rheum. Dis. https://doi.org/10.1136/ard-2022-222881 (2023).
Google Scholar
Hong, M. et al. Fusobacterium nucleatum aggravates rheumatoid arthritis through FadA-containing outer membrane vesicles. Cell Host Microbe 31, 798–810.e7 (2023).
Google Scholar
Chen, J. et al. An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Med. 8, 43 (2016).
Google Scholar
Thompson, K. N. et al. Alterations in the gut microbiome implicate key taxa and metabolic pathways across inflammatory arthritis phenotypes. Sci. Transl. Med. 15, eabn4722 (2023).
Google Scholar
Zhang, X. et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat. Med. 21, 895–905 (2015).
Google Scholar
Breban, M. et al. Faecal microbiota study reveals specific dysbiosis in spondyloarthritis. Ann. Rheum. Dis. 76, 1614–1622 (2017).
Google Scholar
Berland, M. et al. Both disease activity and HLA-B27 status are associated with gut microbiome dysbiosis in spondyloarthritis patients. Arthritis Rheumatol. 75, 41–52 (2023).
Google Scholar
Tito, R. Y. et al. Brief report: dialister as a microbial marker of disease activity in spondyloarthritis. Arthritis Rheumatol. 69, 114–121 (2017).
Google Scholar
Stoll, M. L. et al. The faecal microbiota is distinct in HLA-B27+ ankylosing spondylitis patients versus HLA-B27+ healthy controls. Clin. Exp. Rheumatol. 41, 1096–1104 (2023).
Google Scholar
Scher, J. U. et al. Decreased bacterial diversity characterizes the altered gut microbiota in patients with psoriatic arthritis, resembling dysbiosis in inflammatory bowel disease. Arthritis Rheumatol. 67, 128–139 (2015).
Google Scholar
Viladomiu, M. et al. IgA-coated E. coli enriched in Crohn’s disease spondyloarthritis promote TH17-dependent inflammation. Sci. Transl. Med. 9, eaaf9655 (2017).
Google Scholar
Holers, V. M. et al. Distinct mucosal endotypes as initiators and drivers of rheumatoid arthritis. Nat. Rev. Rheumatol. 20, 601–613 (2024).
Google Scholar
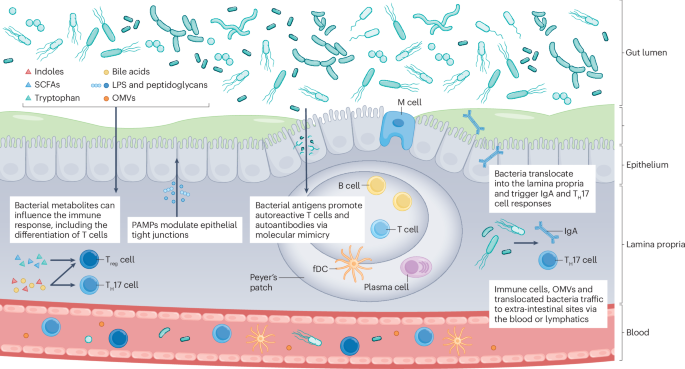
Zaiss, M. M., Joyce Wu, H.-J., Mauro, D., Schett, G. & Ciccia, F. The gut–joint axis in rheumatoid arthritis. Nat. Rev. Rheumatol. 17, 224–237 (2021).
Google Scholar
Gracey, E. et al. Revisiting the gut-joint axis: links between gut inflammation and spondyloarthritis. Nat. Rev. Rheumatol. 16, 415–433 (2020).
Google Scholar
Saha, K., Zhou, Y. & Turner, J. R. Tight junction regulation, intestinal permeability, and mucosal immunity in gastrointestinal health and disease. Curr. Opin. Gastroenterol. 41, 46–53 (2025).
Google Scholar
Tajik, N. et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat. Commun. 11, 1995 (2020).
Google Scholar
Audo, R. et al. Rheumatoid arthritis is associated with increased gut permeability and bacterial translocation that are reversed by inflammation control. Rheumatology 62, 1264–1271 (2023).
Ciccia, F. et al. Dysbiosis and zonulin upregulation alter gut epithelial and vascular barriers in patients with ankylosing spondylitis. Ann. Rheum. Dis. 76, 1123–1132 (2017).
Google Scholar
Singh, A. P. et al. Enteropathogenic E. coli effectors EspF and Map independently disrupt tight junctions through distinct mechanisms involving transcriptional and post-transcriptional regulation. Sci. Rep. 8, 3719 (2018).
Google Scholar
Pradhan, S. et al. Tissue responses to Shiga toxin in human intestinal organoids. Cell Mol. Gastroenterol. Hepatol. 10, 171–190 (2020).
Google Scholar
Kuhn, K. A. et al. Bacteroidales recruit IL-6-producing intraepithelial lymphocytes in the colon to promote barrier integrity. Mucosal Immunol. 11, 357–368 (2018).
Google Scholar
Ey, B., Eyking, A., Gerken, G., Podolsky, D. K. & Cario, E. TLR2 mediates gap junctional intercellular communication through connexin-43 in intestinal epithelial barrier injury. J. Biol. Chem. 284, 22332–22343 (2009).
Google Scholar
Wang, W., Xia, T. & Yu, X. Wogonin suppresses inflammatory response and maintains intestinal barrier function via TLR4-MyD88-TAK1-mediated NF-κB pathway in vitro. Inflamm. Res. 64, 423–431 (2015).
Google Scholar
Abraham, C., Abreu, M. T. & Turner, J. R. Pattern recognition receptor signaling and cytokine networks in microbial defenses and regulation of intestinal barriers: implications for inflammatory bowel disease. Gastroenterology 162, 1602–1616.e1606 (2022).
Google Scholar
Kuhn, K. A., Manieri, N. A., Liu, T. C. & Stappenbeck, T. S. IL-6 stimulates intestinal epithelial proliferation and repair after injury. PLoS ONE 9, e114195 (2014).
Google Scholar
Akuzum, B. & Lee, J. Y. Context-dependent regulation of type17 immunity by microbiota at the intestinal barrier. Immune Netw. 22, e46 (2022).
Google Scholar
Patnaude, L. et al. Mechanisms and regulation of IL-22-mediated intestinal epithelial homeostasis and repair. Life Sci. 271, 119195 (2021).
Google Scholar
Ciccia, F. et al. Type 3 innate lymphoid cells producing IL-17 and IL-22 are expanded in the gut, in the peripheral blood, synovial fluid and bone marrow of patients with ankylosing spondylitis. Ann. Rheum. Dis. 74, 1739–1747 (2015).
Google Scholar
Ciccia, F. et al. Interleukin-9 overexpression and Th9 polarization characterize the inflamed gut, the synovial tissue, and the peripheral blood of patients with psoriatic arthritis. Arthritis Rheumatol. 68, 1922–1931 (2016).
Google Scholar
Jubair, W. K. et al. Modulation of inflammatory arthritis in mice by gut microbiota through mucosal inflammation and autoantibody generation. Arthritis Rheumatol. 70, 1220–1233 (2018).
Google Scholar
Hecquet, S. et al. Increased gut permeability and intestinal inflammation precede arthritis onset in the adjuvant-induced model of arthritis. Arthritis Res. Ther. 25, 95 (2023).
Google Scholar
Matei, D. E. et al. Intestinal barrier dysfunction plays an integral role in arthritis pathology and can be targeted to ameliorate disease. Med. 2, 864–883.e9 (2021).
Google Scholar
Seethaler, B. et al. Biomarkers for assessment of intestinal permeability in clinical practice. Am. J. Physiol. Gastrointest. Liver Physiol. 321, G11–G17 (2021).
Google Scholar
Fasano, A. Zonulin, regulation of tight junctions, and autoimmune diseases. Ann. N. Y. Acad. Sci. 1258, 25–33 (2012).
Google Scholar
Camilleri, M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut 68, 1516–1526 (2019).
Google Scholar
Ayyappan, P. et al. Heightened levels of antimicrobial response factors in patients with rheumatoid arthritis. Front. Immunol. 11, 427 (2020).
Google Scholar
Ajamian, M., Steer, D., Rosella, G. & Gibson, P. R. Serum zonulin as a marker of intestinal mucosal barrier function: may not be what it seems. PLoS ONE 14, e0210728 (2019).
Google Scholar
Bas, S., Gauthier, B. R., Spenato, U., Stingelin, S. & Gabay, C. CD14 is an acute-phase protein. J. Immunol. 172, 4470–4479 (2004).
Google Scholar
Kim, M., Fevre, C., Lavina, M., Disson, O. & Lecuit, M. Live imaging reveals listeria hijacking of E-Cadherin recycling as it crosses the intestinal barrier. Curr. Biol. 31, 1037–1047.e1034 (2021).
Google Scholar
Knoop, K. A., McDonald, K. G., Kulkarni, D. H. & Newberry, R. D. Antibiotics promote inflammation through the translocation of native commensal colonic bacteria. Gut 65, 1100–1109 (2016).
Google Scholar
Lapthorne, S., Macsharry, J., Scully, P., Nally, K. & Shanahan, F. Differential intestinal M-cell gene expression response to gut commensals. Immunology 136, 312–324 (2012).
Google Scholar
Manfredo Vieira, S. et al. Translocation of a gut pathobiont drives autoimmunity in mice and humans. Science 359, 1156–1161 (2018).
Google Scholar
Gronke, K. et al. Translocating gut pathobiont Enterococcus gallinarum induces TH17 and IgG3 anti-RNA–directed autoimmunity in mouse and human. Sci. Transl. Med. 17, eadj6294 (2025).
Google Scholar
Jochum, L. & Stecher, B. Label or concept — what is a pathobiont? Trends Microbiol. 28, 789–792 (2020).
Google Scholar
Allert, S. et al. Candida albicans-induced epithelial damage mediates translocation through intestinal barriers. mBio 9, e00915–e00918 (2018).
Google Scholar
Asquith, M., Elewaut, D., Lin, P. & Rosenbaum, J. T. The role of the gut and microbes in the pathogenesis of spondyloarthritis. Best. Pract. Res. Clin. Rheumatol. 28, 687–702 (2014).
Google Scholar
Gill, T. et al. Axial spondyloarthritis patients have altered mucosal IgA response to oral and fecal microbiota. Front. Immunol. 13, 965634 (2022).
Google Scholar
Akdis, C. A. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat. Rev. Immunol. 21, 739–751 (2021).
Google Scholar
Fine, R. L., Manfredo Vieira, S., Gilmore, M. S. & Kriegel, M. A. Mechanisms and consequences of gut commensal translocation in chronic diseases. Gut Microbes 11, 217–230 (2020).
Google Scholar
Macpherson, A. J. & Uhr, T. Induction of protective IgA by intestinal dendritic cells carrying commensal bacteria. Science 303, 1662–1665 (2004).
Google Scholar
Rescigno, M. et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat. Immunol. 2, 361–367 (2001).
Google Scholar
Spadoni, I., Fornasa, G. & Rescigno, M. Organ-specific protection mediated by cooperation between vascular and epithelial barriers. Nat. Rev. Immunol. 17, 761–773 (2017).
Google Scholar
Spadoni, I. et al. A gut-vascular barrier controls the systemic dissemination of bacteria. Science 350, 830–834 (2015).
Google Scholar
Balmer, M. L. et al. The liver may act as a firewall mediating mutualism between the host and its gut commensal microbiota. Sci. Transl. Med. 6, 237ra266 (2014).
Geva-Zatorsky, N. et al. Mining the human gut microbiota for immunomodulatory organisms. Cell 168, 928–943.e11 (2017).
Google Scholar
Viaud, S. et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science 342, 971–976 (2013).
Google Scholar
Nakamoto, N. et al. Gut pathobionts underlie intestinal barrier dysfunction and liver T helper 17 cell immune response in primary sclerosing cholangitis. Nat. Microbiol. 4, 492–503 (2019).
Google Scholar
Zeng, M. Y. et al. Gut microbiota-induced immunoglobulin G controls systemic infection by symbiotic bacteria and pathogens. Immunity 44, 647–658 (2016).
Google Scholar
Maldarelli, G. A. et al. IgG-seq identifies immune-reactive enteric bacteria in Crohn’s disease with spondyloarthritis. Gut Microbes 17, 2464221 (2025).
Google Scholar
Mårdh, P. A., Nilsson, F. J. & Bjelle, A. Mycoplasmas and bacteria in synovial fluid from patients with arthritis. Ann. Rheum. Dis. 32, 319–325 (1973).
Google Scholar
Chen, T. et al. Bacterial components in the synovial tissue of patients with advanced rheumatoid arthritis or osteoarthritis: analysis with gas chromatography-mass spectrometry and pan-bacterial polymerase chain reaction. Arthritis Care Res. 49, 328–334 (2003).
Google Scholar
Zhao, Y. et al. Detection and characterization of bacterial nucleic acids in culture-negative synovial tissue and fluid samples from rheumatoid arthritis or osteoarthritis patients. Sci. Rep. 8, 14305 (2018).
Google Scholar
Hammad, D. B. M., Liyanapathirana, V. & Tonge, D. P. Molecular characterisation of the synovial fluid microbiome in rheumatoid arthritis patients and healthy control subjects. PLoS ONE 14, e0225110 (2019).
Google Scholar
Chriswell, M. E. et al. Clonal IgA and IgG autoantibodies from individuals at risk for rheumatoid arthritis identify an arthritogenic strain of Subdoligranulum. Sci. Transl. Med. 14, eabn5166 (2022).
Google Scholar
Yang, Y. et al. Within-host evolution of a gut pathobiont facilitates liver translocation. Nature 607, 563–570 (2022).
Google Scholar
Maeda, Y. et al. Mucosal innate immune activation as the trigger to Prevotella species-induced arthritis in genetically resistant mice. Preprint at bioRxiv https://doi.org/10.1101/2025.03.18.643707 (2025).
Kuhn, K. A. & Stappenbeck, T. S. Peripheral education of the immune system by the colonic microbiota. Semin. Immunol. 25, 364–369 (2013).
Google Scholar
Jeong, Y. et al. Therapeutic potential of a novel bifidobacterium identified through microbiome profiling of RA patients with different RF levels. Front. Immunol. 12, 736196 (2021).
Google Scholar
Koh, A., De Vadder, F., Kovatcheva-Datchary, P. & Bäckhed, F. From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165, 1332–1345 (2016).
Google Scholar
Ornelas, A., Dowdell, A. S., Lee, J. S. & Colgan, S. P. Microbial metabolite regulation of epithelial cell-cell interactions and barrier function. Cells 11, 944 (2022).
Google Scholar
He, J. et al. Intestinal butyrate-metabolizing species contribute to autoantibody production and bone erosion in rheumatoid arthritis. Sci. Adv. 8, eabm1511 (2022).
Google Scholar
Rosser, E. C. et al. Microbiota-derived metabolites suppress arthritis by amplifying aryl-hydrocarbon receptor activation in regulatory B cells. Cell Metab. 31, 837–851.e10 (2020).
Google Scholar
Martinsson, K., Dürholz, K., Schett, G., Zaiss, M. M. & Kastbom, A. Higher serum levels of short-chain fatty acids are associated with non-progression to arthritis in individuals at increased risk of RA. Ann. Rheum. Dis. 81, 445–447 (2022).
Google Scholar
Paine, A. et al. Dysregulation of bile acids, lipids, and nucleotides in psoriatic arthritis revealed by unbiased profiling of serum metabolites. Arthritis Rheumatol. 75, 53–63 (2023).
Google Scholar
Lucas, S. et al. Short-chain fatty acids regulate systemic bone mass and protect from pathological bone loss. Nat. Commun. 9, 55 (2018).
Google Scholar
Asquith, M. et al. Intestinal metabolites are profoundly altered in the context of HLA–B27 expression and functionally modulate disease in a rat model of spondyloarthritis. Arthritis Rheumatol. 69, 1984–1995 (2017).
Google Scholar
Dürholz, K. et al. Dietary short-term fiber interventions in arthritis patients increase systemic SCFA levels and regulate inflammation. Nutrients 12, 3207 (2020).
Google Scholar
Häger, J. et al. The role of dietary fiber in rheumatoid arthritis patients: a feasibility study. Nutrients 11, 2392 (2019).
Google Scholar
Agus, A., Planchais, J. & Sokol, H. Gut microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe 23, 716–724 (2018).
Google Scholar
Roager, H. M. & Licht, T. R. Microbial tryptophan catabolites in health and disease. Nat. Commun. 9, 3294 (2018).
Google Scholar
Bansal, T., Alaniz, R. C., Wood, T. K. & Jayaraman, A. The bacterial signal indole increases epithelial-cell tight-junction resistance and attenuates indicators of inflammation. Proc. Natl Acad. Sci. USA 107, 228–233 (2010).
Google Scholar
Alexeev, E. E. et al. Microbiota-derived indole metabolites promote human and murine intestinal homeostasis through regulation of interleukin-10 receptor. Am. J. Pathol. 188, 1183–1194 (2018).
Google Scholar
Scott, S. A., Fu, J. & Chang, P. V. Microbial tryptophan metabolites regulate gut barrier function via the aryl hydrocarbon receptor. Proc. Natl Acad. Sci. USA 117, 19376–19387 (2020).
Google Scholar
Moulin, D. et al. Counteracting tryptophan metabolism alterations as a new therapeutic strategy for rheumatoid arthritis. Ann. Rheum. Dis. 83, 312–323 (2024).
Google Scholar
Stoll, M. L. et al. Fecal metabolomics in pediatric spondyloarthritis implicate decreased metabolic diversity and altered tryptophan metabolism as pathogenic factors. Genes. Immun. 17, 400–405 (2016).
Google Scholar
Berlinberg, A. J. et al. Multi ‘omics analysis of intestinal tissue in ankylosing spondylitis identifies alterations in the tryptophan metabolism pathway. Front. Immunol. 12, 587119 (2021).
Google Scholar
Zelante, T. et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity 39, 372–385 (2013).
Google Scholar
Ye, X. et al. Dual role of indoles derived from intestinal microbiota on human health. Front. Immunol. 13, 903526 (2022).
Google Scholar
Seymour, B. J. et al. Microbiota-dependent indole production stimulates the development of collagen-induced arthritis in mice. J. Clin. Investig. 134, e167671 (2023).
Google Scholar
Ridlon, J. M., Kang, D. J., Hylemon, P. B. & Bajaj, J. S. Bile acids and the gut microbiome. Curr. Opin. Gastroenterol. 30, 332–338 (2014).
Google Scholar
Nieminen, P. et al. Metabolomics of synovial fluid and infrapatellar fat pad in patients with osteoarthritis or rheumatoid arthritis. Inflammation 45, 1101–1117 (2022).
Google Scholar
Coras, R. et al. Baseline microbiome and metabolome are associated with response to ITIS diet in an exploratory trial in patients with rheumatoid arthritis. Clin. Transl. Med. 12, e959 (2022).
Google Scholar
Lefferts, A. R., Norman, E., Claypool, D. J., Kantheti, U. & Kuhn, K. A. Cytokine competent gut-joint migratory T cells contribute to inflammation in the joint. Front. Immunol. 13, 932393 (2022).
Google Scholar
Galván-Peña, S., Zhu, Y., Hanna, B. S., Mathis, D. & Benoist, C. A dynamic atlas of immunocyte migration from the gut. Sci. Immunol. 9, eadi0672 (2024).
Google Scholar
Bradley, C. P. et al. Segmented filamentous bacteria provoke lung autoimmunity by inducing gut-lung axis Th17 cells expressing dual TCRs. Cell Host Microbe 22, 697–704.e4 (2017).
Google Scholar
Dubash, S. et al. Emergence of severe spondyloarthropathy-related entheseal pathology following successful vedolizumab therapy for inflammatory bowel disease. Rheumatology 58, 963–968 (2018).
Diaz, L. I. et al. Vedolizumab-induced de novo extraintestinal manifestations. Gastroenterol. Hepatol. 16, 75–81 (2020).
Naskar, D., Teng, F., Felix, K. M., Bradley, C. P. & Wu, H.-J. J. Synthetic retinoid AM80 ameliorates lung and arthritic autoimmune responses by inhibiting T follicular helper and Th17 cell responses. J. Immunol. 198, 1855–1864 (2017).
Google Scholar
Esplugues, E. et al. Control of TH17 cells occurs in the small intestine. Nature 475, 514–518 (2011).
Google Scholar
Lee, Y. et al. Induction and molecular signature of pathogenic TH17 cells. Nat. Immunol. 13, 991–999 (2012).
Google Scholar
Ghoreschi, K. et al. Generation of pathogenic TH17 cells in the absence of TGF-β signalling. Nature 467, 967–971 (2010).
Google Scholar
Brockmann, L. et al. Intestinal microbiota-specific Th17 cells possess regulatory properties and suppress effector T cells via c-MAF and IL-10. Immunity 56, 2719–2735.e7 (2023).
Google Scholar
Schnell, A. et al. Stem-like intestinal Th17 cells give rise to pathogenic effector T cells during autoimmunity. Cell 184, 6281–6298.e23 (2021).
Google Scholar
He, C. et al. Gut-licensed β7+ CD4+ T cells contribute to progressive retinal ganglion cell damage in glaucoma. Sci. Transl. Med. 15, eadg1656 (2023).
Google Scholar
Krebs, C. F. et al. Autoimmune renal disease is exacerbated by S1P-receptor-1-dependent intestinal Th17 cell migration to the kidney. Immunity 45, 1078–1092 (2016).
Google Scholar
Teng, F. et al. Gut microbiota drive autoimmune arthritis by promoting differentiation and migration of Peyer’s patch T follicular helper cells. Immunity 44, 875–888 (2016).
Google Scholar
Lee, J.-Y. et al. The transcription factor KLF2 restrains CD4+ T follicular helper cell differentiation. Immunity 42, 252–264 (2015).
Google Scholar
Fan, T. et al. Aberrant T follicular helper cells generated by TH17 cell plasticity in the gut promote extraintestinal autoimmunity. Nat. Immunol. 26, 790–804 (2025).
Google Scholar
Breitfeld, D. et al. Follicular B helper T cells express Cxc chemokine receptor 5, localize to B cell follicles, and support immunoglobulin production. J. Exp. Med. 192, 1545–1552 (2000).
Google Scholar
Cinamon, G. et al. Sphingosine 1-phosphate receptor 1 promotes B cell localization in the splenic marginal zone. Nat. Immunol. 5, 713–720 (2004).
Google Scholar
Sun, W. K. et al. Expression of T follicular helper lymphocytes with different subsets and analysis of serum IL-6, IL-17, TGF-β and MMP-3 contents in patients with rheumatoid arthritis. Eur. Rev. Med. Pharmacol. Sci. 23, 61–69 (2019).
Google Scholar
Khunsri, T. et al. Activation of circulating TFH17 cells associated with activated naive and double negative 2 B cell expansion, and disease activity in systemic lupus erythematosus patients. Arthritis Res. Ther. 26, 159 (2024).
Google Scholar
Zhao, J. et al. Increased circulating Tfh17 and PD-1+Tfh cells are associated with autoantibodies in Hashimoto’s thyroiditis. Autoimmunity 51, 352–359 (2018).
Google Scholar
Che, Y. et al. Circulating memory T follicular helper subsets, Tfh2 and Tfh17, participate in the pathogenesis of Guillain-Barré syndrome. Sci. Rep. 6, 20963 (2016).
Google Scholar
Morita, R. et al. Human blood CXCR5+CD4+ T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity 34, 108–121 (2011).
Google Scholar
Klein, L., Kyewski, B., Allen, P. M. & Hogquist, K. A. Positive and negative selection of the T cell repertoire: what thymocytes see (and don’t see). Nat. Rev. Immunol. 14, 377–391 (2014).
Google Scholar
Lycke, N. Y. & Bemark, M. The regulation of gut mucosal IgA B-cell responses: recent developments. Mucosal Immunol. 10, 1361–1374 (2017).
Google Scholar
Mazzini, E., Massimiliano, L., Penna, G. & Rescigno, M. Oral tolerance can be established via gap junction transfer of fed antigens from CX3CR1+ macrophages to CD103+ dendritic cells. Immunity 40, 248–261 (2014).
Google Scholar
Stephens, W. Z. et al. Epithelial-myeloid exchange of MHC class II constrains immunity and microbiota composition. Cell Rep. 37, 109916 (2021).
Google Scholar
Eshleman, E. M. et al. Intestinal epithelial HDAC3 and MHC class II coordinate microbiota-specific immunity. J. Clin. Invest. 133, e162190 (2023).
Google Scholar
Palm, N. W. et al. Immunoglobulin A coating identifies colitogenic bacteria in inflammatory bowel disease. Cell 158, 1000–1010 (2014).
Google Scholar
Demoruelle, M. K. et al. Antibody responses to citrullinated and noncitrullinated antigens in the sputum of subjects with rheumatoid arthritis and subjects at risk for development of rheumatoid arthritis. Arthritis Rheumatol. 70, 516–527 (2018).
Google Scholar
Kinslow, J. D. et al. Elevated IgA plasmablast levels in subjects at risk of developing rheumatoid arthritis. Arthritis Rheumatol. 68, 2372–2383 (2016).
Google Scholar
Bhuyan, Z. A. et al. Genetically encoded Runx3 and CD4+ intestinal epithelial lymphocyte deficiencies link SKG mouse and human predisposition to spondyloarthropathy. Clin. Immunol. 247, 109220 (2023).
Google Scholar
Regner, E. H. et al. Functional intraepithelial lymphocyte changes in inflammatory bowel disease and spondyloarthritis have disease specific correlations with intestinal microbiota. Arthritis Res. Ther. 20, 149 (2018).
Google Scholar
Yao, Y. et al. Short-chain fatty acids regulate B cells differentiation via the FFA2 receptor to alleviate rheumatoid arthritis. Br. J. Pharmacol. 179, 4315–4329 (2022).
Google Scholar
Zhai, Y. et al. Cysteine carboxyethylation generates neoantigens to induce HLA-restricted autoimmunity. Science 379, eabg2482 (2023).
Google Scholar
Kyriakidi, M., Vetsika, E. K., Fragoulis, G. E., Tektonidou, M. & Sfikakis, P. P. Identification and clinical correlation of circulating MAIT, γδ T, ILC3, and pre-inflammatory mesenchymal cells in patients with rheumatoid arthritis and spondyloarthritis. Mediterr. J. Rheumatol. 35, 312–315 (2024).
Google Scholar
Koppejan, H. et al. Altered composition and phenotype of mucosal-associated invariant T cells in early untreated rheumatoid arthritis. Arthritis Res. Ther. 21, 3 (2019).
Google Scholar
Kim, M. et al. TNFɑ and IL-1β in the synovial fluid facilitate mucosal-associated invariant T (MAIT) cell migration. Cytokine 99, 91–98 (2017).
Google Scholar
Nagafuchi, Y. et al. Enhanced gut homing receptor expression of unswitched memory B cells in rheumatoid arthritis. Clin. Exp. Rheumatol. 35, 354–355 (2017).
Google Scholar
Gracey, E. et al. IL-7 primes IL-17 in mucosal-associated invariant T (MAIT) cells, which contribute to the Th17-axis in ankylosing spondylitis. Ann. Rheum. Dis. 75, 2124–2132 (2016).
Google Scholar