Patients
Between June 2020 and April 2022, 131 hips in 122 consecutive patients who received primary DAA-THA with anterior capsular suture at our institute were prospectively enrolled in this study. Patients whose intraoperative hip laxity could not be evaluated were excluded (lack of data [n = 3], fluoroscopy trouble [n = 2], anterior capsules were detached intraoperatively [n = 3]). Two rheumatoid arthritis patients were also excluded due to possible weakness of the joint capsule. Finally, 121 hips in 112 patients were included in the study. The estimated sample size was calculated with G power 3.1 (Heinrich Heine University, Düsseldorf, Germany), and the required number of cases was 35 with effect size of 0.5, α = 0.05, and power of 0.8.
The mean age of patients was 64.7 ± 10.1 years; there were 35 hips in 32 men and 86 hips in 80 women. Mean body mass index was 23.5 ± 3.2 kg/m2. Underlying diseases included: osteoarthritis of the hip in 99 hips in 92 patients; osteonecrosis of the femoral head in 17 hips in 15 patients; and rapidly destructive coxarthropathy in 5 hips in 5 patients. The Crowe classification was used to assess the degree of upward displacement of the femoral head for dysplasia11. The number of hips with type I, II, III, and IV was 72, 21, 6, and 0, respectively. The implants were PINNACLE acetabular cup (DepuySynthes, Warsaw, IN, USA) in 94 hips; Trident hemispherical shell (Stryker, Kalamazoo, MI, USA) in 27 hips; Corail stem (DepuySynthes, Warsaw, IN, USA) in 101 hips; Accolade II (Stryker, Kalamazoo, MI, USA) in 18 hips; and GS Taper stem (Teijin Nakashima Medical, Okayama, Japan) in 2 hips. In all cases ceramic heads and flat polyethylene liners were used. The head sizes were 36 mm, 32 mm, and 28 mm in 36, 78, and 7 hips, respectively. The surgeons basically chose PINNACLE acetabular cup and Corail stem, and other implants were used at the surgeon’s discretion depending on preoperative planning.
Surgical procedure
All patients underwent the same surgical procedure conducted by two senior surgeons with a normal operating table. Both surgeons had conducted DAA-THA in more than 100 cases before this study. All surgeries were performed under a combination of general and epidural anesthesia. The patient was placed in the supine position, and a longitudinal skin incision of approximately 8–10 cm was made peripherally from approximately 2 cm distally and 2 cm laterally from the anterior superior iliac spine. After exposing the anterior capsule, a triangular flap based on the femoral attachment was created (Fig. 1A); the capsular incision was made to preserve the vertical band of the iliofemoral ligament. The flap was inverted to the peripheral side to perform intra-articular manipulation (Fig. 1B). The cup was normally placed in the original position with an inclination of 40° and an anteversion of 15° based on the functional pelvic plane using fluoroscopy or CT-based navigation system (Stryker, Kalamazoo, MI, USA). Subsequently, superolateral release was performed to elevate the femur and insert the stem, while the short external rotators of the hip were typically preserved. The stem was inserted according to the preoperative plan, allowing the anteversion angle of the stem to go from 20° to 30°, and the leg length and global offset were adjusted to the opposite hip as close as possible. After implantation and before suturing anterior capsule, it was checked in all cases that there was no anterior dislocation at 20° of extension and maximum external rotation of the hip. Subsequently, capsular suture was performed at the proximal side with modified Kessler suture and interrupted suture using No. 5 Ethibond Excel (Ethicon, Bridgewater, NJ, USA), and interrupted suture was performed in the remaining parts (Fig. 1C). In 3 of the 6 cases, it was difficult to suture the anterior capsule to the original position. In these cases, the femoral anterior capsular attachment was partially dissected to increase the mobility of capsule and the anterior capsule sutured to the soft tissue near the pelvic capsular attachment and the vertical band of iliofemoral ligament.
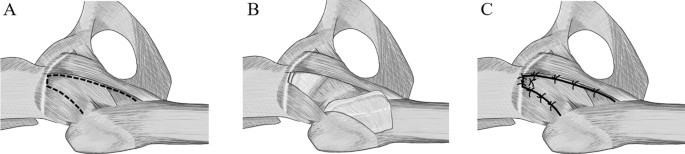
(A) The anterior capsule was incised in a triangular shape (dashed line) to preserve the base of the femoral side of the capsule (right hip shown). (B) The incised flap-shaped anterior capsule was inverted to peripheral side, and manipulation was performed into the joint. (C) After implant insertion, the flap-shaped anterior capsule was returned, and the proximal remnant and the flap were tightly sutured. Then, 3 or 4 sutures were placed on the medial side, and the lateral side was sutured with 2 or 3 stiches.
Method of hip laxity assessment against axial traction
After implantation and before suturing anterior capsule, the ankle band (Smith & Nephew, Watford, UK) which is used for ankle arthroscopy was attached to the ankle joint with the operating table completely flat, and the position of the artificial head before traction was recorded in the antero-posterior view of the hip under fluoroscopy (Fig. 2A). Subsequently, a spring scale (Shinwa Rules Co. Ltd., Niigata, Japan) was used to pull 15 kg to the distal direction (Fig. 3), and the images were recorded likewise (Fig. 2B). This manipulation was performed at the intermediate and 10° extension positions of the hip with neutral rotation and 0° of abduction twice each. The reason for evaluating at extension position is the risk position of anterior dislocation in cases of anterior capsular dissection12. After anterior capsular suture the images were recorded using the same method (Fig. 2C). Regarding traction force, in a cadaver study, the average for opening the joint space by 6 mm was 183 N when the anterior capsule of the native hip was incised by 4 cm9. Thus, the axial traction force was set to 15 kg in this study.
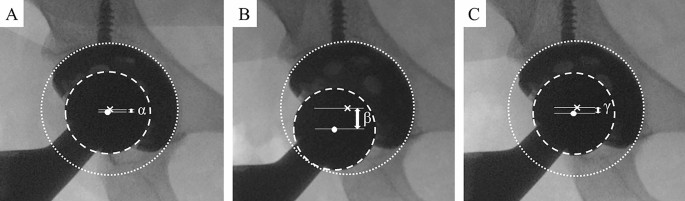
The dotted line is the circle along the cup. The dashed line is the circle along the head. The X mark and white dot represent the center of the cup and head, respectively. The distance between the lines parallel to the bilateral inter-teardrop line passing through these marks was defined as center-head distance (CHD: arrow at both ends). CHD without traction before the capsular suture is α (A), CHD with traction before the capsular suture is β (B), and CHD with traction after the capsular suture is γ (C). Head transfer distance (HTD) before the suture = β – α, HTD after the suture = γ – α, distance controlled by the suture (DCS) = HTD before the suture – HTD after the suture.

An ankle band was placed to the patient’s ankle joint, and traction was applied at 15 kg to the axial direction along the lower limb using spring scale. Antero-posterior views of the hip with and without traction were taken by fluoroscopy in the hip intermediate and 10° extension positions before and after the suture.
With respect to analysis, vertical distance between the center of the cup and head on the image was measured using the image analysis software, IC measure (The imaging source Co., Ltd., Taipei, Taiwan). The actual head size was used to calibrate the head size on the image. The value was defined as the cup-head center distance (CHD). In addition, the value obtained by subtracting CHD before traction from CHD during hip traction was defined as head transfer distance (HTD). CHD and HTD were expressed as the mean value calculated from two images of each. The value obtained by subtracting HTD after suturing anterior capsule from HTD before the suture was considered the distance controlled by the suture (DCS) (Fig. 2). These measurements were performed by two examiners who were not involved in the medical treatment, and average values were used in this study. Intraclass correlation coefficient (ICC) was calculated on 30 randomly selected cases to confirm the reproducibility of the measurements. The measurement for intra-examiner error was conducted at least four weeks apart. ICCs for inter-examiner error and intra-examiner error were 0.994 and 0.996, respectively.
HTD before and after the suture were compared to determine the effect of the suture on hip laxity after DAA-THA.
Measurement of leg length and global offset
Using the antero-posterior view of radiographic images, leg length was measured as the distance of lesser trochanter from the bilateral inter-teardrop line. The global offset was measured as the distance between the pubic symphysis and the long axis of the proximal femur. The values were corrected with calibration markers of 3 cm diameter placed on near the hip. Both measures were taken immediately before and two weeks after surgery. The value obtained by subtracting the preoperative value from the postoperative value in the surgical side was defined as the change in leg length or global offset. Postoperative leg length discrepancy which was the value obtained by subtracting the contralateral side from surgical side was evaluated. The correlations between each value and HTD before the suture at the hip intermediate and 10° extension positions were evaluated.
Statistical analysis
A paired t-test was used to compare HTD before and after anterior capsular suture at the hip intermediate and 10° extension positions. Spearman’s rank correlation coefficient was used to calculate the correlation between HTD before capsular suture and DCS, and between HTD before the suture and the change in leg length or global offset. The values were shown as mean ± standard deviation. p < 0.05 was considered statistically significant. All analyses were performed using GraphPad Prism version 8 (GraphPad, San Diego, CA, USA).
Ethics statement
The study was conducted according to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee and Institutional Review Board at our institute (H2020-068–2). All patients were informed about the study and informed consent was obtained from all participants.


