Rheumatoid Arthritis (RA) is a debilitating chronic inflammatory disease characterized by symmetrical inflammation and erosion of small and large joints, leading to joint damage, severe pain and loss of function1. Extra-articular manifestations and comorbidities are also present in RA, leading to increased morbidity and premature mortality2,3,4,5. In the last few years, increasing emphasis has been placed on the role of RA and its impact on the physical, psychological, and social domains, impairing health-related quality of life. Anxiety and depression have been shown to be associated with increased disease activity and poorer quality of life6,7,8.
In this disease spectrum, chronic pain is a cornerstone symptom of musculoskeletal disorders and has significant predictive value regarding the course of the disease, the degree of disability, the frequency of healthcare utilization, and the socioeconomic and occupational consequences9,10.
In response to chronic pain, patients have adopted a maladaptive coping strategy that involves a misperception of pain through qualitatively negative emotional and cognitive processes: pain catastrophizing (PC), an inclination to exaggerate in describing pain, to ruminate, or to feel helplessness about it11. The term catastrophizing was formally introduced by Albert Ellis and later adopted by Aaron Beck to refer to a maladaptive cognitive process originally described as a peculiar feature of patients with anxiety disorders or depressive disorders. It was based on the principle of an irrational negative anticipation of future events; when applied to present or potential painful experiences, this principle translates into a set of cognitive and emotional patterns that induce the individual to experience an amplified sense of threat and an inability to devise coping strategies6,7,8,9,10,11,12,13.
The most commonly used psychometric tools in clinical practice for defining catastrophizing are the Coping Strategy Questionnaire (CSQ) and the Pain Catastrophizing Scale (PCS). The CSQ includes a subscale consisting of six items related to dimensions of helplessness and pessimism associated with pain. The domains investigated by the PCS are three: Rumination, Magnification, and Helplessness. Rumination refers to the frequent recurrence of thoughts related to experienced pain and the suffering it generates; attention is also focused on the desire for the painful condition to end. Magnification, on the other hand, involves an amplified sense of danger that the pain will worsen or that other adverse events will occur. Helplessness, finally, is a domain that refers to an irrational belief that there is no solution or hope for improvement in the painful experience6,7,8,9,10,11,12,13,14,15.
In several studies, Pain Catastrophizing has been associated to an increased burden of the disease, with higher levels of pain, psychological disability, functional impairment, and poorer quality of life16,17,18.
Furthermore, the proportion of catastrophizing patients remains substantially unchanged when comparing groups of patients with RA, axial spondyloarthritis (axSpA) and Psoriatic Arthritis (PsA), highlighting the importance and prevalence of this maladaptive cognitive perception of pain in different rheumatic diseases7,8,17,18,19,20,21,22. Moreover, other studies conducted in patients with PsA, as well as in those with chronic pain-related rheumatologic conditions such as osteoarthritis, fibromyalgia, and axSpA have confirmed the significant impact of pain catastrophizing on disease burden, psychological distress, and quality of life7,23,24.
Despite its association with subjective disease perception (pain characteristic), PC does not align with inflammation biomarkers, such as swollen joint count, C-Reactive Protein serum level and ultrasound arthritis measures25. Furthermore, in RA patients PC impacts the drug retention rate; high levels of pain catastrophizing reduced the likelihood of achieving composite score remission25,26,27.
In this context, it is possible that patients’ perception of disease and psychological status could reduce the likelihood for achieving remission in RA and PsA7,21,22.
However, nowadays the intricate pathways and mechanisms underlying this reciprocal influence between pain and biological, psychological and social factors remain not entirely elucidated, although different hypothesis have been postulated.
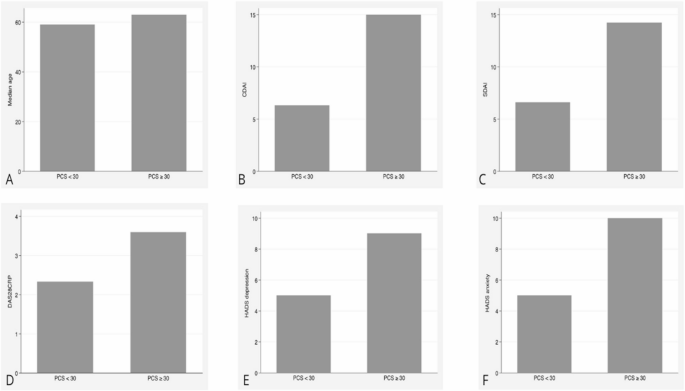
This study aims to explore the relationship between pain catastrophizing and disease activity in RA patients, by analyzing its specific domains, as assessed by the PCS. Furthermore, in the same participants, we analysed if this association is related or not with those psychometric domains which have been related to the catastrophization in patients with chronic pain. By clarifying whether pain catastrophizing correlates with disease severity independently of inflammatory markers, the study seeks to provide clinically meaningful insights for patient stratification and management.