Rheumatoid Arthritis flares are one of the most misunderstood – and most debilitating – parts of this disease.
A flare is not “just a bad day.” It’s not you being dramatic. It’s a surge of immune-driven inflammation that rapidly increases pain, stiffness, swelling, and fatigue. In short, its a period of increased RA symptoms, that are temporary, but very disabling.
This guide explains what RA flares really are, how they behave, what triggers them, how long they last, and how to manage them – using both medical evidence and the lived reality of patients like us.
What Is a Rheumatoid Arthritis Flare? (The Real Definition)
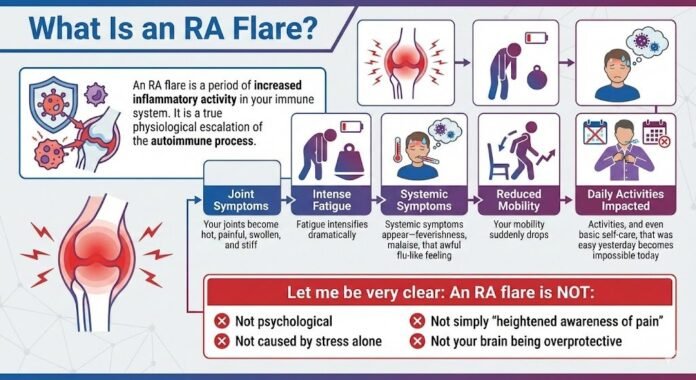
An RA flare is a period of increased inflammatory activity in your immune system. During a flare:
- Your joints become hot, painful, swollen, and stiff
- Fatigue intensifies dramatically
- Systemic symptoms appear – feverishness, malaise, that awful flu-like feeling
- Your mobility suddenly drops
- Activities that were easy yesterday become impossible today
Let me be very clear: An RA flare is not psychological. It’s not caused by stress alone. It’s not simply “heightened awareness of pain” or your brain being overprotective.
It is a true physiological escalation of the autoimmune process.

Common Symptoms of an RA Flare
RA flares typically include some combination of:
Severe joint pain:
Deep, hot, throbbing pain, often affecting multiple joints at once.
Sudden increase in stiffness:
Especially morning stiffness that lasts far longer than usual.
Visible swelling:
Your joints may look red, feel warm, or appear visibly enlarged.
Extreme fatigue:
Worse than your “baseline” RA fatigue. This is body-shutting-down exhaustion.
Feverish or flu-like feelings:
This reflects your immune system ramping up.
Reduced mobility:
Simple tasks like opening jars, walking, or getting dressed become difficult or impossible.
Emotional strain:
This is not the cause of flares…it’s the consequence of them.
How Long Do RA Flares Last?
Flare duration varies, but most fall into three categories:
Mini-flares (hours to 1-2 days):
Often linked with overuse, weather shifts, or minor immune fluctuations.
Standard flares (a few days to a few weeks):
These require rest, symptom management, and sometimes medication adjustments.
Major or persistent flares (weeks to months):
These indicate uncontrolled disease activity and require medical intervention.
A flare is considered clinically significant if it lasts more than 48 hours or impacts your mobility and function.
What Causes RA Flares? (Real Triggers vs Myths)
RA flares are caused by immune activation, but the trigger isn’t always clear.
Here are some proven or widely recognized triggers:
Underlying disease activity:
The most common cause. Your RA is active and needs stronger treatment.
Infections:
Viral infections are a major trigger because they activate your immune system. COVID, flu, RSV, even a common cold.
Weather changes:
Barometric pressure drops, humidity shifts, cold weather. Yes, this is real.
Overuse or physical exertion beyond your current tolerance:
Exercise is generally great for RA long-term, but it’s easy to overdo it.
Stress:
Stress may cause flares in some people, but this isn’t true for everyone. If stress does trigger flares for you, it’s important to work on stress reduction and management techniques.
Missed medications or medication wearing off:
Some RA medications have unpleasant side effects, and it’s tempting to skip a dose or take a “medication holiday.” But this can destabilize your treatment and cause your disease to flare.
Hormonal changes:
Menstrual cycles, perimenopause, postpartum periods.
Surgical procedures or vaccinations:
Temporary immune activation can trigger flares.
Sleep deprivation:
Poor sleep increases cytokine activity.
What Flares Are NOT Caused By:
- Catastrophizing
- Negative thinking
- Not “managing your mindset”
- Fear of movement
- Personality traits
Your immune system is driving a flare. Not your personality.
How to Know If It’s a Flare or Disease Progression
Flares come and go. But if a flare does NOT go away—if the increased pain and fatigue stretch into weeks or even months—it’s time to make an appointment with your rheumatologist to adjust your treatment plan.
Signs it’s a flare:
- Symptoms spike suddenly
- Pain and stiffness vary by day
- Swelling increases then decreases
- Function returns between episodes
Signs of progression:
- Symptoms creep up gradually over months
- Daily function keeps decreasing
- Joints become permanently stiff
- Imaging shows erosions or synovial thickening
If you’re unsure, you’re not alone. But when in doubt, it’s always worth a call to your rheumatologist.
Managing an RA Flare: What Actually Helps
A good flare plan has four pillars:
1. Rest (Actual Rest, Not “Just Take It Easy”)
During a flare, your immune system is in overdrive. Rest is not optional—it is physiological relief.
Rest helps reduce cytokine activity and protects inflamed joints. You’re not being lazy. You’re managing active inflammation.
2. Heat or Cold Therapy
- Heat for stiffness
- Cold for swelling or intense pain
Different joints may need different approaches. Experiment and see what works for you.
3. Medications Used During Flares
This is educational information, not medical advice, but common tools include:
- NSAIDs for pain and swelling
- Prednisone or prednisolone (short bursts to tame inflammation)
- Adjusting DMARD dosing (under doctor supervision)
- Biologics or JAK inhibitors if flares are frequent
Here’s the thing: frequent flares indicate insufficient disease control. Not personal failing. If you’re having frequent flares, its time to make an appointment with your rheumatologist.
4. Pacing & Activity Modification
Lower your expectations during a flare:
- Break tasks into smaller steps
- Prioritize essential tasks only
- Reduce physical load
- Ask for help (you’re not weak—you’re inflamed)
When to Call Your Doctor
You should seek medical review if:
- A flare is very severe and/or lasts longer than 7 days
- You develop a fever not explained by RA
- Swelling becomes severe or new joints are involved
- You cannot bear weight
- Flares are happening monthly or more
Flares are a sign that inflammation is not controlled and you need a change to your management plan.
The Emotional Toll of RA Flares (Rarely Acknowledged)
Flares are frightening and destabilizing. They disrupt:
- Work
- Relationships
- Sleep
- Independence
- Identity
Many patients feel guilt, shame, or fear of judgment because RA is invisible. Some ignorant people may suggest you’re exaggerating the pain or making it up. Some people lack empathy and will likely never understand.
None of this is your fault.
A flare is a disease event, not a character flaw.
Why Some People Have More Flares Than Others
Several factors influence flare frequency:
- Seropositive vs seronegative RA
- Genetics
- Comorbidities (like MCTD, AS, Lupus, Hashimoto’s)
- Underlying disease activity
- Medication effectiveness
- Infections
- General health and fitness
- Sleep quality
- Hormones
Frequent flares mean you deserve better disease control, not a lecture.
Can You Prevent Flares?
Not entirely, but you may be able to reduce them by:
- Maintaining consistent treatment and following your rheumatologist’s plan
- Avoiding known triggers
- Pacing activity
- Keeping sleep as stable as possible
- Managing infections promptly
- Using DMARDs/biologics adequately
- Eating a healthy, nutritious diet
Some people flare rarely. Some flare often.
Neither pattern is your fault.
FAQ About RA Flares
Can a flare cause permanent damage?
A single flare is unlikely to cause permanent damage if your RA is generally well-controlled. But frequent, severe flares over time can lead to joint damage. That’s why it’s so important to work with your rheumatologist to reduce flare frequency.
Should I exercise during a flare?
Gentle movement might help with stiffness once the worst of the inflammation settles, but during the acute phase of a severe flare, rest is more important. Listen to your body. If it hurts to move, don’t push through it.
Why do my flares seem random?
Sometimes they are. Your immune system doesn’t send you a memo before it decides to ramp up inflammation. But tracking your flares over time might reveal patterns—weather, stress, hormones, or other triggers.
Will flares get worse over time?
Not necessarily. With proper treatment, many people experience fewer and less severe flares over time. But if your flares are getting worse or more frequent, that’s a sign your treatment needs adjustment.
Is it normal to feel scared during a flare?
Absolutely. Flares are unpredictable and can be severe. It’s normal to feel anxious about when the next one will hit or how bad it will be. This is a rational response to living with an unpredictable disease and/or being in severe, uncontrolled pain.