Stimulated by Shi et al 2025.[1]
LDH – lumbar disc herniation
RCT – randomised controlled trial
VAS – visual analogue scale
JOA – Japanese Orthopaedic Association score for low back pain
SIJ – sacroiliac joint
SR – systematic review
GRADE – Grading of Recommendations, Assessment, Development and Evaluation (a method of grading the quality or ‘certainty’ and strength or ‘effect size’ of evidence in healthcare)– key to acronyms
This is a moderately large RCT from a well-known hospital in Beijing, which is part of the China Academy of Chinese Medical Sciences.
240 patients with LDH were randomised and allocated equally to 4 treatment groups (n=60 per group): acupuncture plus manipulation; acupuncture alone; manipulation alone; lumbar traction. The trial was open, but the data collection and statistical analysis was blinded.
Treatments were applied 3 times a week for 3 weeks and patients were followed up at 3 months. Outcomes were VAS pain and JOA score, and these were measured at baseline, week 1, week 3, 1 month follow-up, and 3 months follow-up.
The JOA score for low back pain was introduced in 1986,[2] following a similar score for cervical myelopathy in 1975.[3] Since those original scores, both have been modified more than once.
This trial uses the original version of the JOA score for low back pain, which ranges from 0 to 29, with higher numbers corresponding to better function. Points are allocated to subjective symptoms (9 points), clinical signs (6 points) and activities of daily living (14 points).
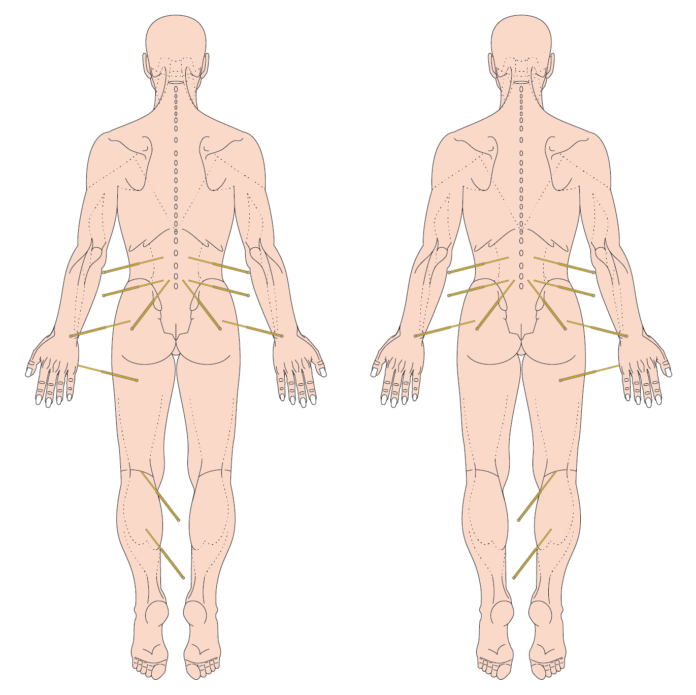
The acupuncture protocol involved bilateral points in the lumbar area and hip girdle and unilateral points on the unaffected side. Jiayi points (presumably at the level affected) – these are one fingerbreadth from the midline and target multifidus. The other numbered points lumbar and hip girdle areas were BL25, BL23, and GB30. The unilateral points used were SI3, BL40, BL57. The needle size used for all points apart from GB30 was 0.25mm diameter and 40mm length. A 60mm needle of the same diameter was used for GB30. Needles were retained for 30 minutes per treatment session.
The manipulation protocol involved 7 different manoeuvres including gentle lumbar mobilisation, acupressure, two different rotational manipulations, SIJ mobilisation, manual traction, and repetitive passive lumbar flexion. The whole session lasted 20-30m minutes.
Traction was applied using a computerised traction bed for 20-30 minutes, starting at 40% body weight and increasing to 50%, unless patients were frail or elderly, in which case they started at 30% and increased to 40% of body weight.
All 4 groups improved significantly from baseline. The acupuncture alone and manipulation alone groups were rather similar, with the combined group unsurprisingly being the best, and the traction group demonstrating the least benefit.
There is no discussion of correction for multiple significance testing and the p<0.05 level seems to have been adopted. ANOVA demonstrated that the combined group was best, and the traction group was worst at this significance level.
It is not really a surprise that the combined group did better with twice the passive intervention time provided to the other groups. I guess we need to consider a cost benefit perspective since the differences between groups were not particularly big. MCID between group means (VAS pain) was only just achieved between the best and worst groups following treatment. Readers will know that I am not a fan of this use of MCID; however, we have no control for natural history in this study, so the traction group has to be used as the comparator instead.
The improvements in this study are comparable to those published in an SR of acupuncture for LDH from 2018 in Acupuncture in Medicine.[4] It included 30 studies from China and a total of 3503 patients. Acupuncture proved to be better than most comparators, but not tuina, in this review. This review was made up of a lot of small open (unblinded) trials for the certainly level (GRADE) was low or very low for all comparisons.
References
1 Shi F, Wen H, Liu Y, et al. Comparative clinical efficacy of acupuncture combined with manipulation and other non-pharmacological interventions in the treatment of lumbar disc herniation: a prospective, multi-arm, randomized, open-label, blinded endpoint trial. Front Med. 2024;11:1507115. doi: 10.3389/fmed.2024.1507115
2 Fukui M, Chiba K, Kawakami M, et al. Japanese Orthopaedic Association Back Pain Evaluation Questionnaire. Part 2. Verification of its reliability : The Subcommittee on Low Back Pain and Cervical Myelopathy Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association. J Orthop Sci. 2007;12:526–32. doi: 10.1007/s00776-007-1168-4
3 Kato S, Oshima Y, Oka H, et al. Comparison of the Japanese Orthopaedic Association (JOA) score and modified JOA (mJOA) score for the assessment of cervical myelopathy: a multicenter observational study. PloS One. 2015;10:e0123022. doi: 10.1371/journal.pone.0123022
4 Tang S, Mo Z, Zhang R. Acupuncture for lumbar disc herniation: a systematic review and meta-analysis. Acupunct Med. 2018;36:62–70. doi: 10.1136/acupmed-2016-011332
Declaration of interests MC
Published