Demographic and clinical characteristics of enrolled RA patients
In this study, 5004 patients were analyzed, with 541 (10.8%) achieving Boolean2.0 remission. The demographic and clinical characteristics of the enrolled RA patients are summarized in Table 1. The median (IQR) age at RA diagnosis of the patients was 51.00 (42.00, 60.00) years, with the majority being female (3978, 79.5%). The median (IQR) disease duration was 26.00 (3.00, 89.00) months, and the median (IQR) follow-up duration after enrollment in the SSDM group was 1.00 (0, 18.00) months.
The patients who achieved Boolean2.0 remission (49.00 [41.00, 58.00] years) were younger than those who did not (51.00 [42.00, 61.00] years) at RA diagnosis. The median (IQR) disease duration was shorter in the remission group (21.00 [2.00, 70.75] months) compared to the non-remission group (27.00 [4.00, 91.00] months), and the median follow-up duration was significantly longer in the remission group (19.00 [7.00, 37.00] months vs. 0 [0, 15.00] months). The duration of morning stiffness was significantly shorter in the group of patients achieving Boolean2.0 remission (P < 0.001). The patients who did not achieve remission had a higher median number of tender joints (5.00 [2.00, 12.00]) than that in the remission group (4.00 [2.00, 9.00]) at the baseline, while the number of swollen joints were comparable.
Patients who achieved Boolean2.0 remission exhibited lower levels of C-reactive protein at the baseline. Furthermore, disease activity scores of RA patients achieving Boolean2.0 remission, including CDAI, SDAI, DAS28-CRP and DAS28-ESR, as well as scores reflecting patient and physician assessments, including PtGA, PhGA, HAQ-DI, were significantly lower at the baseline (all P < 0.001).
Treatment comparison of RA patients categorized by Boolean2.0 remission
Treatment strategies of enrolled RA patients are illustrated in Table 2. Methotrexate (2259, 45.1%) and leflunomide (2202, 44.0%) were the most common csDMARDs administered, following by hydroxychloroquine (1027, 20.5%). The frequency of JAKi (134, 2.7%) and TNFi (161, 3.2%) were relatively low for our RA patients when enrolled in the SSDM. Besides, glucocorticoids (800, 16.0%) and NSAIDs (1009, 20.2%) were also administered to patients as adjunctive therapy. Among patients who achieved Boolean2.0 remission, a higher percentage were prescribed with methotrexate (292 [54.0%] vs. 1967 [44.1%]), and leflunomide (267 [49.4%] vs. 1935 [43.4%]). Conversely, a lower percentage of patients were treated with JAKi (5 [0.9%] vs. 129 [2.9%]) or glucocorticoids (62 [11.5%] vs. 738 [16.5%]).
Therapeutic regimens were further explored, which were divided into 5 categories, including csDMARD monotherapy, combination therapy with two csDMARDs, three or more csDMARDs combination, TNFi combination with csDMARDs, and JAKi combination with csDMARDs. A higher percentage of patients achieved Boolean2.0 remission received combination therapy with two csDMARDs (185 [34.2%] vs. 1040 [23.3%]) whereas a lower percentage administered with JAKi and csDMARDs combination (3 [0.6%] vs. 106 [2.4%]) when compared with patients not achieved remission.
Predictors of Boolean2.0 remission in enrolled RA patients
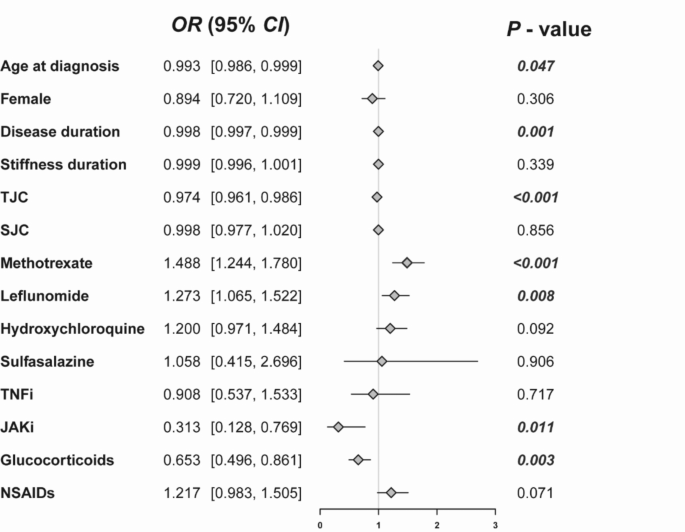
To explore the predictors of Boolean2.0 remission, logistic analyses were further carried out. The results of univariate logistic analysis were illustrated in Fig. 1. Younger age at RA diagnosis, shorter disease duration, lower number of tender joints were positively related to remission. As for treatment strategies, treatment with methotrexate and leflunomide were related to remission, while glucocorticoids and JAKi were related to non-remission (all P < 0.05).
Univariate logistic analysis to analyze the predictive factors of achieving Boolean2.0 remission in RA patients. Values highlighted in bold represent statistically significant P values (P < 0.05). NSAIDs, non-steroidal anti-inflammatory drugs; JAKi, janus kinase inhibitors; OR, odds ratio; SJC, swollen joint count; TNFi, tumor necrosis factor inhibitors; TJC, tender joint count.
Multivariate analysis was further performed to analyze the predictive factors of achieving Boolean2.0 remission in RA patients (Fig. 2). The likelihood of being in remission was higher in patients with younger age, shorter disease duration, lower number of tender joints, methotrexate and leflunomide prescription (all P < 0.05).
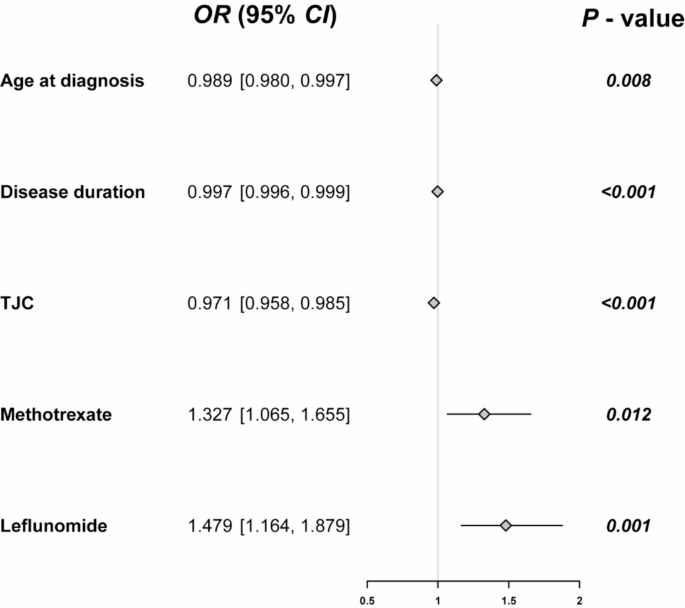
Multivariate logistic analysis to analyze the predictive factors of achieving Boolean2.0 remission in RA patients. Values highlighted in bold represent statistically significant P values (P < 0.05). OR, odds ratio; TJC, tender joint count.
Subgroup analysis between different groups based on age
As age was one of risk factors for Boolean2.0 remission, we further explored the clinical characteristics in different age groups. The cut-off point of age (61.5 years) at diagnosis was determined with ROC curves (high Youden index).
In total of 720 patients were 61.5 years or older when diagnosed with RA, among whom 77 (10.7%) patients achieved Boolean2.0 remission (Table 3). In the group of patients with 61.5 years or older, the median follow-up duration was significantly longer in the remission group (19.00 [9.00, 30.50] months vs. 1.00 [0, 20.00] months). The patients who did not achieve remission had a significantly higher median number of tender joints (9.00 [4.00, 18.00]) than that in the remission group (5.00 [3.00, 13.00]) at the baseline. Patients who achieved Boolean2.0 remission exhibited lower levels of inflammatory index, including C-reactive protein and erythrocyte sedimentation rate at the baseline. Furthermore, disease activity scores of RA patients achieving Boolean2.0 remission, including CDAI, SDAI, DAS28-CRP and DAS28-ESR, as well as scores reflecting patient and physician assessments, including PtGA, PhGA, HAQ-DI, were significantly lower at the baseline (all P < 0.001). In terms of treatment regimen, methotrexate (306, 42.5%) and leflunomide (334, 46.4%) were the most common administered DMARDs, and compared to patients not in remission, patients in remission had relatively higher rates of methotrexate and leflunomide usage. Furthermore, a higher percentage of patients achieved Boolean2.0 remission were prescribed with two csDMARDs combination therapy compared to non-remission patients (30 [39.0%] vs. 155 [24.1%]).
Among 4282 patients younger than 61.5 years, 464 (10.8%) patients attained Boolean2.0 remission (Table 4). The median (IQR) age at RA diagnosis was 48.00 (39.00, 54.00) years, with the majority being female (3447, 81.2%). Compared to non-remission patients, the median disease duration (25.00 [2.00, 82.00] months vs. 36.00 [6.00, 120.00] months) and stiffness duration (2.50 [0.00, 30.00] minutes vs. 9.00 [0.00, 30.00] minutes) were shorter whereas follow-up duration was significantly longer (18.50 [7.00, 38.00] months vs. 0.00 [0, 15.00] months) in the remission group. Patients who achieved Boolean2.0 remission exhibited lower number of tender joints and lower levels of C-reactive protein at the baseline. Furthermore, disease activity scores of RA patients achieving Boolean2.0 remission, including CDAI, SDAI, DAS28-CRP and DAS28-ESR, as well as scores reflecting patient and physician assessments, including PtGA, PhGA, HAQ-DI, were significantly lower at the baseline (all P < 0.001). With respect to medications, patients in remission group had relatively higher rates of methotrexate, leflunomide and NSAIDs, and lower rates of JAKi and glucocorticoids usage. Further exploration about treatment regimen showed that a higher percentage of patients achieved Boolean2.0 remission received combination therapy with two csDMARDs than that in non-remission groups (165 [35.6%] vs. 960 [25.1%]).