The Clinical and Laboratory Evidence
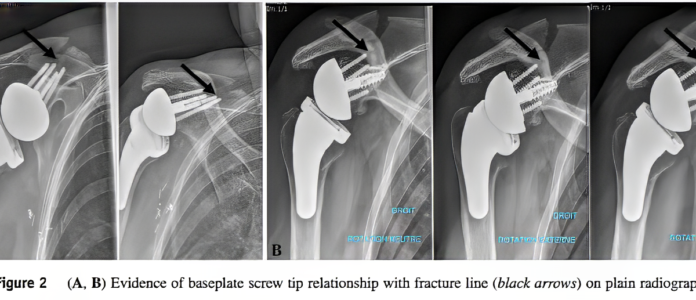
Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: an analysis of 485 consecutive cases reported: “we found that 57.1% of the scapular spine fractures (12 of 21) occurred at the distal tip of the superior screw”
Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification found “Of 16 scapular spine fractures, 14 occurred from a screw tip.”
Scapula fractures after reverse total shoulder arthroplasty: classification and treatment: “We no longer recommend placing the most superior screw for metaglene fixation because this appears to lead to a potential stress riser that may contribute to this fracture of the scapular spine”
Scapular spine base fracture with long outside-in superior or posterior screws with reverse shoulder arthroplasty: an in vitro study reported “The main finding of the study was that when the superior metaglene screw (with or without a posterior or anterior screw) enters into the base of the spine with an outside-in configuration, it leads to a fracture at the base of the scapular spine compared to the short screw “not touching the scapula spine” group.”

This leads to some interesting questions:
(1) Is it the screw or the hole?
The evidence is that putting a short screw into a too-long hole doesn’t reduce the weakening of the bone. The hole is the problem. Leaving the drilled hole incompletely filled may actually worsen the weakening of the scapular spine. Even “appropriate length” screws that don’t breach the cortex may still weaken the spine if the drill hole penetrates into the spine base.
(2) Which screw hole is the one to worry about?
We often say “go short on drilling the superior hole”. I took a look at the scapular model that lives on my desk. As we see, the spine is not directly superior, but rather posterior-superior.

From this we recognize that the “worry hole” may not be the superior hole (12 o’clock) but rather a posterior-superior hole (10:30 for right shoulder, 1:30 for left shoulder) depending on how the baseplate is rotationally oriented on the prepared glenoid (see diagram of a left shoulder below in which the red trapezoid represents the position of the scapular spine and, for the baseplate orientation in the middle figure, the “worry hole” is at 1:30).

(3) How important are the superior screws?
We took a look at this question in the post “Learning from baseplate failure”, noting that most failed baseplates fail by rocking into superior tilt.

This is because the rocking moment is applied to the inferior aspect of the glenosphere.

This rocking moment (red) is resisted by compression of the upper baseplate against the reamed bone (yellow) and resistance to pullout by the central and inferior screws (green).

When this stabilization mechanism fails, the gleosphere rocks up and out. Note that the superior screw is not in a position to resist this rocking.

So how important is the superior screw?
The Fixation Hierarchy
Tier 1 – Essential (Contribute Most to Preventing Clinical Failure)
Inferior screws: Resist the rocking moment that causes baseplate failure; I go long on these.
Tier 2 – Important (When Safe Trajectories Available)
Anterior screws: Contribute meaningfully to fixation with low fracture risk- usually can safely maximize length of bone hole and screw length.
Tier 3 – Optional/Risk-Benefit Consideration
Positioned near center of rocking loosening, contribute minimally to preventing superior rocking (the dominant failure mode)
Are associated with 40-70% of scapular spine fractures when trajectory enters spine base
I “short” the drill hole in the “worry holes”, or in small patients leave them out all together.
Conclusion:
Central fixation dominates – A long central screw engaging far cortex provides 60-70% of baseplate stability.
Inferior screws prevent the failure mode that most commonly occurs – Since baseplates usually fail by rocking superiorly with inferior screw pullout, I maximize inferior screw purchase to directly address the clinical failure mechanism.
Posterior/Superior screws create risk without proportional benefit – They contribute 8-12% to total fixation but minimal resistance to superior tilt, while contributing to 40-70% of spine fractures when drill trajectories penetrate the spine base.
Maximize fixation where it prevents clinical failure (central, inferior), minimize risk where it doesn’t (spine-directed trajectories). This requires intraoperative anatomic judgment based on actual baseplate position.
As we noted in our recent post on preventing acromial/scapular spine fractures, this represents another surgeon-controlled variable in a multifactorial problem. Combined with appropriate humeral positioning, CAL preservation when possible, and judicious glenosphere selection, selective screw strategy can help minimize these challenging complications.
It’s about holes

Red-Breasted Sapsucker
Washington Park Arboretum
2020
Here are some videos that are of shoulder interest
Shoulder arthritis – what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link)
The total shoulder arthroplasty (see this link)
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).