In his classic paper, Morphologic study of the glenoid in primary glenohumeral osteoarthritis, Gilles Walch identified the B1 and B2 glenoids as being common of types of arthritic glenohumeral pathoanatomy in patients presenting for anatomic shoulder arthroplasty.
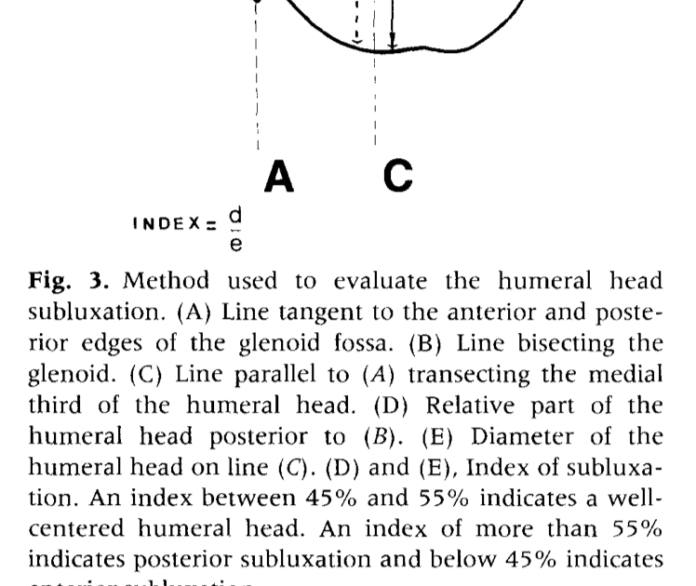
An important characteristic of these glenoid types is the posterior decentering of the humeral head on the glenoid, a critical element in the evaluation and management of glenohumeral arthritis. Note that the degree of decentering was (and remains) defined by the relationship of the humeral head to the face of the glenoid (and not the plane of the scapula), as seen from this figure from his classic article.
The decentering of the head on the glenoid can be evaluated on the standardized axillary “truth” view, as shown in the five examples below.

By the “truth” view, we mean an axillary view obtained with the arm elevated in the plane of the scapula that shows the spinoglenoid notch or “eye” (red arrow) as shown in this Steve Lippitt illustration:

The rationale for evaluating decentering with the arm elevated to a functional position is that CTs or MRIs obtained with the arm at the side may not reveal it, as shown in the two images of the same shoulder shown below. The MRI obtained with the arm at the side does not reveal decentering, whereas dramatic posterior decentering is shown when the arm is elevated to a functional position in the axillary “truth” view.

While often considered together, the B1 and B2 are not the same. The B1 has posterior decentering of the humerus on the glenoid without biconcavity of the glenoid from bony erosion. By contrast, the B2 has posterior decentering of the humeral head on the glenoid with biconcavity of the glenoid as shown in these illustrations from the classic article by Walch.

A third B was added by the authors of A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging.

As can be seen from these figures, the B3 is monoconcave (i.e. no biconcavity) with substantial retroversion and without posterior decentering of the humeral head on the glenoid, i.e. the humeral head is centered with respect to the glenoid.
This point is emphasized by the authors of Quantitative measurement of bony pathology in advanced glenohumeral osteoarthritis who use the term “humeral-glenoid alignment (HGA)” to indicate centering or decentering of the humeral head on the glenoid. HGA is measured as the position of the humeral head center relative to the perpendicular line drawn from the glenoid center point (without reference to the scapular axis). This relationship is shown in a figure from their article showing the centering of the humeral head in a B3 glenoid (i.e. the humeral head is not decentered).

(1) implant loosening (26.1%), with 21.7% of failures attributed to glenoid component loosening.
(2) Rotator cuff insufficiency (17.3%).
(3) Instability (10.4%)
The most common reasons for revision in the AOA experience were instability/dislocation (31.1%), rotator cuff insufficiency (24.2%), and loosening/lysis and implant breakage glenoid insert (11.0% each). The most common reasons in Kaiser experience were rotator cuff tear (32.3%), glenoid component loosening (29.0%), and dislocation and infection (12.9% each).
While these articles did not study the relationship of glenoid type to loosening or instability, we can venture that because B1 and B2 glenoids demonstrate preoperative posterior decentering, they would be at risk for postoperative instability. The B3, being centered preoperatively would seem less at risk for instability as long as the centering was not disrupted by the arthroplasty.
B1 – conservative reaming without attempting to alter version, preserving glenoid bone stock, excellent carpentry to assure perfect seating of the component, and use of an anteriorly eccentric humeral head to manage excessive posterior translation if that is evident on intraoperative examination with a concentric trial humeral head component in place.
B2 – conservative reaming – just sufficient to convert the biconcavity to a mono concavity without attempting to alter glenoid version, preserving glenoid bone stock, excellent carpentry to assure perfect seating of the component, and use of an anteriorly eccentric humeral head to manage excessive posterior translation if that is evident on intraoperative examination with a concentric trial humeral head component in place.
B3 – conservative reaming without attempt to alter glenoid version, preserving glenoid bone stock, excellent carpentry to assure perfect seating of the component. An anteriorly eccentric humeral head component is rarely necessary because of the absence of preoperative decentering.
For additional information on this approach see:
Pollination

Bumble Bee on Iris
Montlake Fill
Spring 2021