Age-related localised deposition of amyloid in connective tissue has been found in degenerative articular and periarticular tissue. Biopsies of the supraspinatus tendon of 28 patients undergoing repair of the rotator cuff were analysed histologically for the presence of localised deposition of amyloid. There was a long history of impingement in 20 patients, and eight patients had suffered an acute traumatic tear with no preceding symptoms. Localised deposition of amyloid identified by Congo Red staining was detected in 16 samples (57%). Amyloid was present in 14 (70%) of the degenerative tears, but in only two (25%) of the acute tears. Immunohistochemical staining showed that the amyloid deposits were positive for P component, but negative for kappa and lambda light chains, prealbumin, and beta2 microglobulin. Critical electrolyte staining revealed highly-sulphated glycosaminoglycans at sites of deposition of amyloid. The presence of localised deposition of amyloid in tears of the rotator cuff is likely to represent irreversible structural changes. These findings support the theory that impingement and tears are due to intrinsic degenerative changes within the tendons of the rotator cuff.
Wininger, A. E., et al. (2021). “Musculoskeletal pathology as an early warning sign of systemic amyloidosis: a systematic review of amyloid deposition and orthopedic surgery.” BMC Musculoskelet Disord 22(1): 51.
BACKGROUND: Transthyretin and immunoglobulin light-chain amyloidoses cause amyloid deposition throughout various organ systems. Recent evidence suggests that soft tissue amyloid deposits may lead to orthopedic conditions before cardiac manifestations occur. Pharmacologic treatments reduce further amyloid deposits in these patients. Thus, early diagnosis improves long term survival. QUESTIONS/PURPOSES: The primary purpose of this systematic review was to characterize the association between amyloid deposition and musculoskeletal pathology in patients with common orthopedic conditions. A secondary purpose was to determine the relationship between amyloid positive biopsy in musculoskeletal tissue and the eventual diagnosis of systemic amyloidosis. METHODS: We performed a systematic review using PRISMA guidelines. Inclusion criteria were level I-IV evidence articles that analyzed light-chain or transthyretin amyloid deposits in common orthopedic surgeries. Study methodological quality, risk of bias, and recommendation strength were assessed using MINORS, ROBINS-I, and SORT. RESULTS: This systematic review included 24 studies for final analysis (3606 subjects). Amyloid deposition was reported in five musculoskeletal pathologies, including carpal tunnel syndrome (transverse carpal ligament and flexor tenosynovium), hip and knee osteoarthritis (synovium and articular cartilage), lumbar spinal stenosis (ligamentum flavum), and rotator cuff tears (tendon). A majority of studies reported a mean age greater than 70 for patients with TTR or AL positive amyloid. CONCLUSIONS: This systematic review has shown the presence of amyloid deposition detected at the time of common orthopedic surgeries, especially in patients >/=70 years old. Subtyping of the amyloid has been shown to enable diagnosis of systemic light-chain or transthyretin amyloidosis prior to cardiac manifestations.
Zhang, D., et al. (2021). “Orthopaedic Manifestations of Amyloidosis.” J Am Acad Orthop Surg 29(10): e488-e496.
Amyloidosis is a disorder of misfolded proteins in human tissues, which can result in morbid cardiac and neurological disease. Historically, the utility of tissue biopsy during orthopaedic procedures to detect amyloidosis has been limited because no disease-modifying therapies were available; however, new drug therapies have recently emerged for the treatment of amyloidosis. Although these novel pharmaceuticals show promise for slowing disease progression, they are primarily effective in the early stages of amyloidosis, underscoring the importance of early diagnosis. Common orthopaedic manifestations of amyloidosis include carpal tunnel syndrome, trigger finger, spontaneous distal biceps tendon rupture, rotator cuff disease, and lumbar spinal stenosis. Carpal tunnel syndrome is frequently the earliest manifestation of amyloidosis, on average preceding a formal diagnosis of amyloidosis by over four years. By recognizing the constellation of musculoskeletal symptoms in the patient with amyloidosis, orthopaedic surgeons can play an active role in patient referral, early detection of systemic disease, and prompt initiation of disease-modifying treatment. There may be a role for selective biopsy for amyloid deposition in at-risk patients during routine orthopaedic procedures.
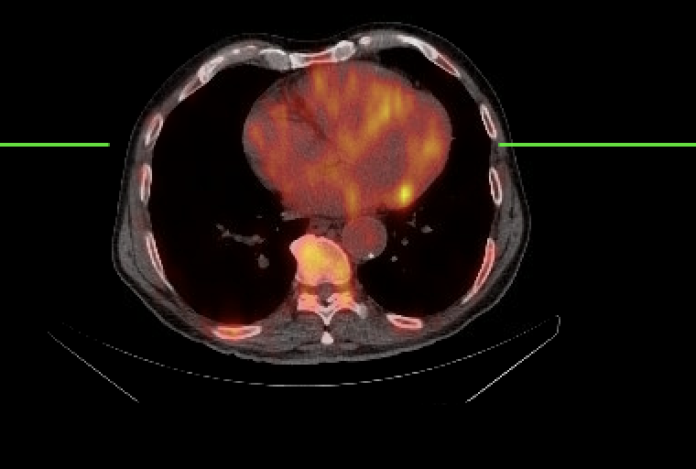
Perfetto, F., et al. (2022). “Transthyretin Cardiac Amyloidosis: A Cardio-Orthopedic Disease.” Biomedicines 10(12).
Orthopaedic manifestations of wild-type transthyretin amyloidosis are frequent and characteristic, including idiopathic bilateral carpal tunnel syndrome, idiopathic lumbar canal stenosis, atraumatic rupture of the brachial biceps tendon, and, more rarely, finger disease and rotator cuff. These manifestations often coexisting in the same patient, frequently male and aged, steadily precede cardiac involvement inducing a rapidly progressive heart failure with preserved ejection fraction. Although transthyretin cardiac amyloidosis remains a cardiac relevant disease, these extracardiac localisation may increase diagnostic suspicion and allow for early diagnosis assuming the role of useful diagnostic red flags, especially in light of new therapeutic opportunities that can slow or stop the progression of the disease. For the cardiologist, the recognition of these extracardiac red flags is of considerable importance to reinforce an otherwise less emerging diagnostic suspicion. For orthopedists and rheumatologists, the presence in an old patient with or without clinical manifestations of cardiovascular disease, of an unexpected and inexplicable constellation of musculoskeletal symptoms, can represent a fundamental moment for an early diagnosis and treatment is improving a patient’s outcome.
Rath, J., et al. (2024). “Carpal Tunnel, Trigger Finger, and Spinal Stenosis: The Rest of the Story.” S D Med 77(11): 516-525.
Amyloidosis is a deadly systemic disease in which misfolded proteins accumulate in human tissue eventually leading to morbid dysfunction in multiple organ systems. The prognosis of untreated amyloidosis is poor. Orthopedic manifestations of amyloidosis include carpal tunnel syndrome (CTS), trigger digit, distal biceps tendon rupture, rotator cuff disease, and lumbar spinal stenosis. These orthopedic conditions are early red flags for systemic amyloidosis. CTS is often the earliest manifestation and can precede the disease by over four years. With the advent of medications that can slow the progression of amyloidosis, particularly in the early stages of the disease, it is imperative to diagnose amyloidosis early on. Both primary care physicians and orthopedic surgeons can recognize the various orthopedic conditions associated with amyloidosis and play a vital role in early disease detection. Awareness of the musculoskeletal presentation of systemic amyloidosis can lead to earlier detection and treatment that can delay the progression of the disease.