Rheumatoid Arthritis (RA) is a systemic autoimmune inflammatory disease. It causes the immune system to mistakenly attack the body’s own tissues, particularly the synovial lining of joints, leading to pain, swelling, stiffness, and, if undertreated, permanent joint damage.
That’s the definition most medical websites give you.
But RA is far more complex – and far more serious – than “just joint pain.” It is a whole-body disease. It affects energy levels, appetite, sleep, mood, circulation, the eyes, the lungs, and even the voice. It’s unpredictable, variable, and incredibly misunderstood.
I’ve lived with inflammatory arthritis for over a decade – RA, MCTD, Ankylosing Spondylitis overlap – and if there’s one truth I want newly diagnosed patients to know, it’s this:
RA is real, physical, inflammatory disease.
It is not a mindset problem. It is not “central sensitisation.”
And it is absolutely not your fault.
This guide brings together clinical science and lived experience to explain what RA really is, how it behaves, and what people with RA wish doctors, family, and policymakers understood.
This guide isn’t written by someone in a white coat who’s never lived it. This combines actual medical science with what it’s really like to have RA.
What Is Rheumatoid Arthritis? (The Simple Version)
Your immune system is supposed to protect you. But with RA, it gets confused and attacks the lining of your joints – the synovium. That’s not a metaphor. That’s what actually happens.
This leads to:
- Chronic inflammation that doesn’t quit
- Pain and stiffness that can be mild or absolutely debilitating
- Joint damage that builds up over time
- Symptoms that go way beyond your joints
And here’s what RA is NOT: It’s not caused by stress. It’s not caused by your personality. It’s not “central sensitisation” or your brain overreacting or any of that nonsense.
It is a real, biological, autoimmune disease.
Key Facts about RA You Need to Know
- RA is autoimmune, not the wear-and-tear arthritis your grandmother had.
- RA causes inflammation. Real, measurable inflammation – not “just pain.”
- Early treatment can prevent joint damage. This matters.
- RA can affect your eyes, lungs, heart, and even your voice.
- The fatigue is real. It’s not laziness. It’s your body fighting itself.
- Symptoms are different for everyone. Your RA won’t look like mine.
- People with RA often look perfectly fine on the outside while feeling absolutely terrible.
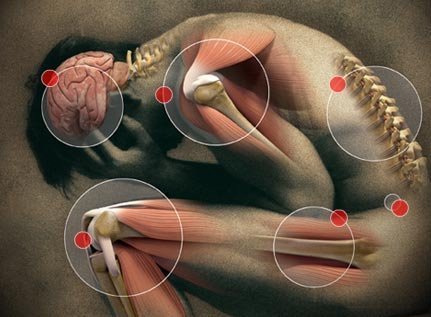
How Rheumatoid Arthritis Affects Your Body
RA usually starts with inflammation in the synovium – that’s the lining of your joints. Your immune system attacks it, and then things spiral:
- The synovium thickens
- Inflammatory fluid builds up
- Your body releases cytokines (TNF, IL-6, IL-1)—these are the chemicals that make everything hurt
- Eventually, your cartilage and bone get damaged
These are biological processes. Real things happening in your body. Yes, pain can be influenced by emotions and stress – I’m not denying that. But the pain from RA is caused by actual pathology. Not your mindset. Not fear. Not some “overprotective brain” theory that makes it sound like you’re imagining things.
RA is a Systemic Disease…Not Just Joint Pain
This is the part people don’t get. RA is systemic. That means it affects your entire body.
Joint symptoms:
- Visible swelling
- Warmth and redness (note: sometimes there is not much swelling or redness, but the pain is still very real)
- Morning stiffness that can last hours
- Limited movement
- Difficulty gripping things or walking
Systemic symptoms:
- Severe fatigue…not tiredness, fatigue. There’s a difference.
- Feverish feeling and general malaise
- Night sweats
- Weight loss when the disease is active
Extra-articular symptoms
- Eye inflammation (iritis/uveitis)
- Lung complications
- Rheumatoid nodules (lumps under your skin)
- Anaemia
- Raynaud’s phenomenon (fingers going white/blue in the cold)
- Voice changes from arthritis in your throat
- TMJ involvement—yes, jaw pain
Internal link opportunities: Symptoms Hub, Raynaud’s, TMJ, Voice, Fatigue.
What Do RA Symptoms Feel Like?
The Pain:
RA pain is inflammatory pain. That means:
- It’s often worse after you’ve been resting
- It’s most often a deep, aching, burning, throbbing pain
- It can be mild, moderate, or severe
- It usually comes with visible swelling or tenderness, although sometimes there is barely any swelling to be seen
Fibromyalgia is common in people with RA. But fibromyalgia pain and RA pain are NOT the same thing. Don’t let anyone dismiss your RA pain as “central sensitisation.” They’re different conditions.
The Flares:
RA flares are episodes where everything gets worse and you may experience:
- Intense inflammation
- Severe pain
- Joint stiffness and weakness
- Profound fatigue
Flares can last hours, days, or weeks. You never know when one’s coming or how long it’ll stick around. That’s what makes them so hard to deal with. Oh, and they are often completely invisible.
Internal link: RA Flares page.
Why RA Looks Different in Different People
This is important. RA has:
- Different onset patterns (some people get hit hard and fast, others develop it slowly)
- Different joints affected
- Different antibody profiles (seropositive vs seronegative)
- Different levels of systemic involvement
That’s why no two people with RA have the exact same symptoms. Your RA will not look like someone else’s RA. And that’s okay.
What Causes RA?
The honest answer is we don’t fully know. But here’s what we do know:
Genetics:
RA has strong genetic links, including something called HLA-DRB1 “shared epitope” genes. If someone in your family has it, you’re at higher risk.
Internal link: Genetics of RA.
Environmental Triggers:
Things that might trigger RA in people who are already genetically susceptible:
- Smoking (this is a big one)
- Silica exposure
- Periodontal disease (gum disease)
- Possibly certain infections
Internal link: Environmental Triggers.
Immune Dysregulation:
Basically, your immune system’s tolerance breaks down and it starts attacking your joint tissues. Why? We’re still figuring that out.
How RA Is Diagnosed
Doctors diagnose RA by looking at several things:
Clinical signs:
- Which joints are swollen and how many
- Pattern of joint involvement
- How long morning stiffness lasts
Blood tests:
- Rheumatoid factor (RF)
- Anti-CCP antibodies
- Inflammatory markers (ESR, CRP)
Here’s something crucial: Seronegative RA is real. That means your blood tests can be negative and you can still have aggressive RA. Don’t let anyone tell you otherwise. Or put your joint pain down to fibromyalgia.
Imaging:
- Ultrasound shows synovitis
- MRI detects early bone marrow edema
- X-rays show later damage
Internal link: RA Diagnosis (future page).
How RA Is Treated
DMARDs (Disease-Modifying Anti-Rheumatic Drugs):
These reduce inflammation and actually prevent joint damage from happening:
- Methotrexate
- Sulfasalazine
- Hydroxychloroquine
- Leflunomide
Internal link: DMARDs page.
Biologic Therapies:
These target specific immune pathways (TNF, IL-6, B-cells). They’re newer and can be incredibly effective.
Internal link: Biologics page.
JAK Inhibitors:
Oral medications for moderate to severe RA. Another option if other treatments don’t work.
Internal link: JAK inhibitors.
Corticosteroids:
Useful for short-term flares. They shouldn’t be used long-term because of serious side effects. But here’s the reality—some people don’t respond to any currently available treatments and are forced to stay on corticosteroids long-term. When that happens, the goal is to use the lowest dose that actually works.
What Patients Need to Know About Treatment
- Early, aggressive treatment leads to the best outcomes. Push for this.
- Many patients are undertreated, especially women. Advocate for yourself.
- Overlapping diseases (RA plus other conditions) make treatment more complex.
- “Treat-to-target” works—but only if doctors actually listen to you.
Living With RA
Good Days and Bad Days:
Symptoms fluctuate. Your function changes daily. That’s normal with RA.
Fatigue Is Not Laziness:
Inflammatory fatigue is a full-body shutdown. It’s not being tired. It’s different.
Internal link: RA Fatigue page.
Exercise Helps – But Maybe Not for the Reasons You’ve Been Told:
Movement reduces inflammation and maintains strength. Period. Not because you’re “retraining your nervous system” or because “pain is in the brain.” Those theories minimize what you’re dealing with.
Internal link: Exercise & RA.
You Are Not Imagining Your Pain:
RA pain comes from inflamed tissues, swollen joints, cytokines, structural compression, and mechanical strain. This is painful.
Period.
The Bottom Line
Rheumatoid Arthritis is a complex, serious medical disease. It affects your joints, your organs, your energy, and your daily function.
But here’s the thing: with the right treatment and the right support, people with RA can live meaningful, fulfilling lives. Those who respond well to medication can live relatively normal lives with a normal life span.
Yes, RA pain can be very severe.
But you are not imagining your symptoms.
You are not exaggerating.
You are not responsible for your disease.
RA is real. It’s caused by inflammation and pathology.
And you deserve real treatment.
RA FAQ
What is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune inflammatory disease where the immune system attacks the joints, causing pain, swelling, stiffness, and fatigue
What are the first signs of RA?
Early symptoms often include morning stiffness, swollen joints in the hands or feet, fatigue, and pain that improves with movement but worsens after rest.
Is RA the same as osteoarthritis?
No. Osteoarthritis is wear-and-tear arthritis. RA is autoimmune inflammation that can damage joints and affect organs throughout the body.
How is Rheumatoid Arthritis diagnosed?
Doctors use blood tests, physical examinations, and imaging such as ultrasound or MRI to confirm RA and assess inflammation and joint involvement.
Can RA be cured?
No cure exists, but RA can be treated effectively with DMARDs, biologics, and targeted therapies that reduce inflammation and prevent joint damage.
Does stress cause RA?
No. Stress may worsen symptoms, but it does not cause RA. RA is driven by immune system dysfunction, not personality or mindset.
What is an RA flare?
A flare is a period of intense inflammation causing worsening pain, swelling, stiffness, and fatigue.
What organs can RA affect?
RA can involve the eyes, lungs, heart, blood vessels, skin, voice box, and more — because it is a systemic disease.